The medical device industry demands an unprecedented convergence of precision, biocompatibility, regulatory compliance, and rapid responsiveness to evolving clinical needs. Vacuum casting, also known as polyurethane casting, has emerged as a transformative manufacturing technology uniquely positioned to meet these demands. This article provides a comprehensive analysis of vacuum casting’s role in medical device development and production, exploring its fundamental processes, material science advancements, key applications across clinical specialties, regulatory considerations, and future trajectories. Through case studies, technical comparisons, and industry insights, we illustrate how vacuum casting bridges the gap between prototyping and low-volume production, accelerates time-to-market, and enables the creation of patient-centric medical solutions. With a focus on real-world implementations and material innovations, this work demonstrates why vacuum casting has become an indispensable tool in modern medical manufacturing.
The global medical device market, valued at over $514 billion in 2023 and projected to exceed $719 billion by 2030 (Grand View Research), is driven by aging populations, technological advancements in minimally invasive procedures, and the growing demand for personalized healthcare. These trends impose stringent requirements on device manufacturers: components must exhibit micron-level precision, withstand sterilization cycles, interact safely with biological tissues, and be produced efficiently to address urgent clinical needs—from pandemic response to chronic disease management.
Traditional manufacturing methods often struggle to balance these priorities.
Injection molding, while ideal for high-volume production, requires substantial upfront investment in metal tooling (typically $10,000–$100,000+) and lengthy lead times (4–12 weeks), making it impractical for early-stage development or low-volume runs.
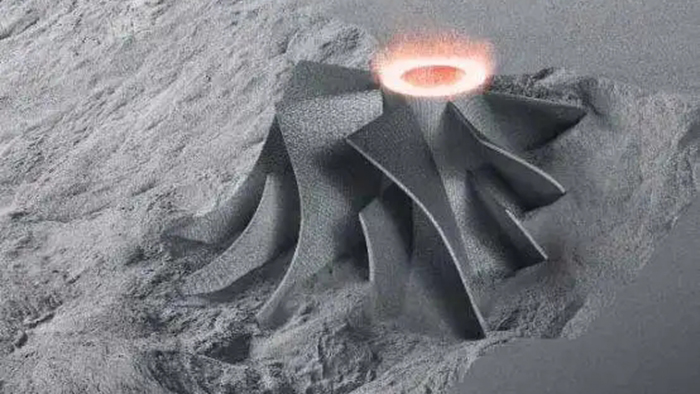
CNC machining, though precise, is cost-prohibitive for complex geometries and limited in material versatility. Additive manufacturing (
3D printing) excels at
rapid prototyping but often fails to replicate the mechanical properties or surface finishes required for end-use medical devices.
Vacuum casting addresses these limitations by combining the precision of molding with the flexibility of rapid manufacturing. Defined as a low-volume casting process that uses silicone molds and liquid polyurethane resins under vacuum conditions to produce high-fidelity parts, it fills a critical niche in the medical manufacturing ecosystem. Unlike injection molding’s metal tooling, vacuum casting relies on silicone molds that can be produced in days rather than weeks, at a fraction of the cost (typically $500–$3,000 per mold) . These molds can replicate intricate details—from microfluidic channels to textured grips—with dimensional accuracy of ±0.05 mm or better , while supporting a wide range of medical-grade materials that mimic the properties of ABS, polypropylene, rubber, and even bioresorbable polymers .
This article aims to provide medical device engineers, product developers, and manufacturing professionals with a holistic understanding of
vacuum casting’s applications in healthcare. Section 2 details the vacuum casting process, from master model creation to post-processing. Section 3 explores the material science of medical-grade resins, emphasizing biocompatibility and sterilization resistance. Section 4 examines key applications across diagnostic equipment, surgical tools, prosthetics, and medical training. Section 5 compares vacuum casting to alternative manufacturing methods. Section 6 addresses regulatory compliance and quality control. Section 7 presents future trends, and Section 8 concludes with practical implementation guidance. Throughout, case studies, technical specifications, and multimedia resources illustrate real-world applications.
At its essence, vacuum casting leverages negative pressure to eliminate air bubbles and ensure complete mold filling—critical for medical devices where even microscopic defects can compromise functionality or biocompatibility . The process operates on a simple yet precise sequence: creating a master model, fabricating a silicone mold, mixing and pouring resin, curing, and finishing. Unlike open-air casting, the vacuum environment prevents porosity, ensuring parts with uniform density and consistent mechanical properties .
The master model is the blueprint for vacuum-cast parts, and its precision directly determines the quality of the final product. Modern master models are typically produced using two technologies:
-
Additive Manufacturing: Stereolithography (SLA) or Selective Laser Sintering (SLS) 3D printing is preferred for complex geometries, as it can create internal channels, undercuts, and fine details with accuracy of ±0.025 mm . For medical applications, SLA printers using biocompatible resins (e.g., Formlabs BioMed Resin) are often used to ensure the master model meets initial regulatory benchmarks.
-
CNC Machining: Ideal for master models requiring ultra-smooth surfaces or made from engineering plastics (e.g., PEEK, ABS). CNC-machined masters are particularly useful for devices like surgical instrument handles, where surface texture directly impacts ergonomics .
Case Example: A leading manufacturer of endoscopes used SLA-printed master models with microscale lens mounts (0.5 mm tolerance) to create vacuum-cast prototypes. This approach reduced master model lead time from 3 weeks (CNC) to 48 hours .
Silicone mold creation is a critical step that balances flexibility and durability. Medical-grade silicone (e.g., Shore A 30–70 hardness) is mixed with a catalyst and poured around the master model in a casting box. The assembly is then placed in a vacuum chamber to remove air bubbles, ensuring the silicone penetrates every detail of the master. After curing (typically 4–24 hours at room temperature or accelerated with heat), the mold is cut along a pre-marked seam to remove the master .
Key Considerations for Medical Molds:
-
Mold Life: Most silicone molds produce 25–50 parts before degradation, though high-quality medical-grade silicone (e.g., Dow Corning Sylgard 184) can yield up to 100 parts .
-
Release Agents: Medical applications require non-toxic, biocompatible release agents (e.g., food-grade silicone sprays) to avoid contaminating cast parts .
-
Undercut Accommodation: Silicone’s flexibility allows for demolding of parts with undercuts (e.g., snap-fit enclosures) without complex mold inserts, a major advantage over injection molding .
Medical-grade resins—primarily polyurethanes, with epoxy and silicone variants—are mixed in precise ratios (typically 1:1 or 2:1 by weight) to achieve desired properties. The mixture is degassed in a vacuum chamber to remove air bubbles, then poured into the silicone mold. The mold is returned to the vacuum chamber to ensure complete filling, even in thin-walled sections (minimum 0.75 mm recommended, 1.5 mm optimal) .
Curing conditions vary by resin type:
-
Room-Temperature Curing: Most polyurethanes cure in 4–8 hours, suitable for prototypes and non-sterile components.
-
Heat-Accelerated Curing: Oven curing (60–80°C) reduces cycle time to 1–2 hours and improves material properties, critical for load-bearing parts like prosthetic components .
After curing, the silicone mold is peeled away to reveal the cast part. Silicone’s flexibility minimizes part damage during demolding, preserving fine details like engraved serial numbers or texture patterns .
Medical devices often require post-processing to meet clinical standards:
-
Trimming: Removing gate marks and flash using precision tools (e.g., scalpel, laser cutter).
-
Surface Treatment: Sanding (up to 2000-grit) for smoothness, or texturing for grip. For diagnostic equipment, polishing to achieve optical clarity (e.g., PMMA-like resins) .
-
Assembly: Integrating electronic components (e.g., sensors in wearable devices) or metal inserts (e.g., stainless steel hinges in surgical tools) .
-
Sterilization Compatibility: Ensuring finishes withstand autoclaving, ethylene oxide (EtO), or gamma radiation (see Section 3.3) .
Table 1 summarizes key technical parameters of vacuum casting for medical applications:
*Source: Compiled from *
Vacuum casting relies heavily on polyurethane (PU) resins due to their tunable properties, biocompatibility, and processability. For medical applications, three primary material categories dominate:
Mimicking engineering plastics like ABS, polycarbonate (PC), and PMMA, these resins offer high strength and dimensional stability. Key examples include:
-
ABS-Like Polyurethanes: (e.g., Materialise RPU 70) Feature impact resistance (Izod notched impact: 20 J/m) and chemical resistance, ideal for device enclosures (e.g., ultrasound probes) .
-
PMMA-Like Resins: (e.g., Smooth-On Crystal Clear 200) Offer optical clarity (transmittance > 90%) for diagnostic components like light guides or microscope parts .
-
PC-Like Resins: (e.g., Henkel Loctite 3D 3843) Provide high heat resistance (Tg = 120°C) for devices requiring autoclaving .
Resembling rubber, TPE, or silicone, these materials are used for seals, gaskets, and patient-contacting components:
-
Rubber-Like Polyurethanes: (e.g., Materialise RPU 40) Exhibit high elongation at break (> 300%) and tear resistance, suitable for surgical instrument grips or prosthetic liners .
-
Silicone Resins: (e.g., Dow Corning SE 1700) Offer biocompatibility and temperature resistance (-60°C to 200°C), used in wound care dressings or catheter components .
Tailored for high-performance medical applications:
-
Bioresorbable Resins: (e.g., Polycaprolactone-based PU) Degrade naturally in the body, under investigation for temporary implants like bone fixation devices .
-
Conductive Resins: (e.g., Carbon-filled PU) Enable electromagnetic shielding for sensitive diagnostic equipment or electrode components in neurostimulation devices .
-
X-Ray Opaque Resins: (e.g., Barium sulfate-filled PU) Allow visualization of devices (e.g., catheters) during imaging procedures .
For any patient-contacting device, biocompatibility is mandatory. Vacuum casting materials must comply with international standards, including:
-
ISO 10993: Evaluates biological response to medical devices, covering cytotoxicity, sensitization, irritation, and systemic toxicity.
-
FDA 21 CFR Part 177: Regulates materials in contact with biological fluids (e.g., blood, tissue).
Case Example: Covestro’s Baymedix® line of polyurethanes includes Baymedix® AP 501 (aliphatic prepolymer) and Baymedix® FP 520 (hydrophilic polyisocyanate), both ISO 10993-certified for wound care and wearable devices. These materials exhibit low skin irritation and high moisture permeability, critical for long-wear patches .
Medical devices must withstand sterilization without degradation. Vacuum-cast materials vary in their compatibility with common sterilization methods:
*Source: *
Engineers must select resins based on sterilization needs. For example, a surgical instrument grip requiring repeated autoclaving would use a high-temperature PC-like resin, while a single-use diagnostic component might use an EtO-compatible ABS-like resin .
Choosing the right resin requires balancing four factors:
-
Clinical Use Case: Implantable vs. external, reusable vs. single-use.
-
Biocompatibility Requirements: ISO 10993-5 (cytotoxicity) for all patient-contacting parts; ISO 10993-4 (hemocompatibility) for blood-contacting devices.
-
Sterilization Method: As per Table 2.
-
Mechanical Properties: Tensile strength (critical for prosthetics), flexibility (seals), or optical clarity (diagnostics).
Example Decision Path: For a reusable endoscope handle—patient-contacting, autoclave-sterilized, requires impact resistance—an ISO 10993-certified, heat-resistant ABS-like polyurethane (e.g., Henkel Loctite 3843) is optimal .

Vacuum casting’s versatility enables its use across virtually every medical specialty. Below are detailed applications, supported by case studies and technical requirements.
Diagnostic devices rely on precision, optical clarity, and electromagnetic shielding—all strengths of vacuum casting.
-
Ultrasound Probe Housings: ABS-like polyurethanes with textured grips and acoustic window inserts (PMMA-like resin) are vacuum-cast to ensure ergonomic handling and signal transmission. Materialise produced vacuum-cast housings for Hoya’s vision simulator system, achieving optical clarity comparable to injection-molded parts while reducing lead time by 60% .
-
Microfluidic Chips: Flexible or rigid resins are used to create microchannels (50–500 μm width) for lab-on-a-chip devices. Vacuum casting ensures uniform channel dimensions, critical for accurate fluid flow in blood analyzers .
PoC devices require portability and low-cost production for distributed healthcare settings. Vacuum casting enables small-batch production of:
-
Test Strip Holders: Rigid ABS-like resins with precise slot dimensions (±0.1 mm) to align test strips with optical sensors.
-
Device Enclosures: Combined with conductive resin inserts for electromagnetic shielding, protecting sensitive electronics in glucose monitors or ECG machines .
Case Study: During the COVID-19 pandemic, Materialise developed a vacuum-cast NIP connector for ventilators in 10 days. Using a rubber-like polyurethane (RPU 40) with high flexibility, the connectors met ISO 13485 standards and helped alleviate shortages in overwhelmed hospitals .
Surgical tools demand precision, durability, and ergonomic design—vacuum casting delivers on all fronts.
-
Grips and Handles: Over-molded parts combining rigid ABS-like cores (structural support) and flexible rubber-like outer layers (ergonomic grip) are produced via vacuum casting. This over-molding capability eliminates assembly steps, reducing cost and improving reliability .
-
Specialized Tips: Fine-tipped instruments (e.g., ophthalmic tools) use vacuum-cast resins with high dimensional accuracy (±0.05 mm) to avoid tissue damage .
For components like trocar seals or catheter guides, vacuum casting offers cost-effective low-volume production:
-
Seals and Gaskets: Silicone-based resins with high chemical resistance to withstand surgical fluids.
-
Disposable Handles: Biodegradable or recyclable PU resins, aligning with sustainability goals .
Vacuum casting enables personalized, patient-specific prosthetic and orthotic devices—critical for comfort and functionality.
-
Socket Liners: Flexible, skin-friendly polyurethanes (e.g., Baymedix® AP 501) are vacuum-cast to match the patient’s residual limb shape, reducing pressure points and improving circulation .
-
Structural Components: Rigid PC-like resins with carbon fiber reinforcement are used for prosthetic feet and knees, offering strength-to-weight ratios comparable to metal .
Case Study: Sunpe Manufacturing produced a vacuum-cast rib cage model for medical simulators using PP-type resin (UP 5690) with over-molded 304 stainless steel supports. The model withstands 1,200 compressions, mimicking real chest compressions for CPR training .
-
Custom Inserts: Vacuum-cast from 3D-scanned foot models, using flexible resins that adapt to gait patterns.
-
Spinal Braces: Rigid outer shells (ABS-like resin) with foam liners (hydrophilic PU) for breathability .
Medical simulation relies on realistic, durable models—vacuum casting excels at replicating anatomical details.
-
Organ Models: Silicone resins with tissue-like texture (e.g., liver, kidney) for surgical training. Vacuum casting reproduces vascular networks and organ contours with high fidelity .
-
Skeletal Models: Rigid PU resins reinforced with fiberglass for durability, used in anatomy courses .
-
Endoscopy Trainers: Transparent PMMA-like resin enclosures with internal structures mimicking the gastrointestinal tract.
-
Injection Simulators: Soft rubber-like resins for skin layers and muscle tissue, allowing trainees to practice needle insertion .
The growing wearable tech market (projected to reach $118 billion by 2028) benefits from vacuum casting’s ability to produce small, complex, patient-friendly components.
-
Biometric Sensors: Miniaturized enclosures (10–20 mm) with precise openings for optical or electrical sensors. Vacuum casting ensures sensor alignment (±0.05 mm) for accurate data collection .
-
Skin-Contact Components: Hydrophilic polyurethanes (e.g., Baymedix® FP 520) that wick moisture, reducing irritation in 24/7 wearables like heart rate monitors .
-
Adhesive Layers: Baymedix® A-series adhesives, which offer variable adhesion strength (removable without skin damage) and can be integrated with drug reservoirs via vacuum casting .
-
Electrode Patches: Conductive resin components for transdermal drug delivery, ensuring uniform current distribution .
To understand vacuum casting’s unique value, it is critical to compare it to competing technologies for medical applications.
Injection molding remains the gold standard for high-volume medical production, but vacuum casting is superior for early-stage and low-volume needs:
*Source: *
Example: A startup developing a new glucose monitor needed 200 prototypes for clinical trials. Vacuum casting ($2,000 tooling, $15 per part = $5,000 total) was 90% cheaper than injection molding ($20,000 tooling, $2 per part = $24,000 total) .
3D printing is ideal for rapid prototyping, but vacuum casting produces higher-quality end-use parts:
*Source: *
Case Example: A manufacturer of surgical guides switched from SLA 3D printing to vacuum casting. The vacuum-cast guides exhibited 30% higher impact resistance and passed 100 autoclave cycles, compared to 20 cycles for 3D-printed parts .
*Source: *
Table 4 provides a framework for choosing between vacuum casting and alternatives:
The medical device industry is one of the most heavily regulated globally, and vacuum casting processes must adhere to strict standards to ensure patient safety.
-
ISO 13485: Quality management system for medical device manufacturers. Requires documentation of all vacuum casting steps, from material sourcing to post-processing .
-
FDA QSR (21 CFR Part 820): U.S. regulation mandating design controls, process validation, and traceability. Vacuum casting molds and resins must be traceable to lot numbers .
-
EU MDR (2017/745): European regulation requiring clinical evidence of safety. Vacuum-cast devices must undergo biocompatibility testing per ISO 10993 .
Regulators require validation that vacuum casting processes consistently produce conforming parts. Key validation steps include:
-
Process Qualification (PQ): Verifying that mold fabrication, resin mixing, and curing parameters meet specifications. For example, validating that a silicone mold produces parts within ±0.1 mm tolerance for 50 consecutive cycles .
-
Material Validation: Testing resins for biocompatibility (ISO 10993) and sterilization resistance before use.
-
Inspection Protocols: Implementing 100% visual inspection for surface defects and statistical process control (SPC) for dimensional accuracy .
-
Dimensional Inspection: Using coordinate measuring machines (CMM) or 3D scanners to verify compliance with CAD models.
-
Material Testing: Tensile strength (per ASTM D638) and elongation tests to ensure mechanical properties.
-
Sterility Testing: Culturing samples post-sterilization to detect microbial contamination (per ISO 11737) .
-
Visual Inspection: Magnification (10–20x) to check for porosity, flash, or surface defects that could harbor bacteria .
Comprehensive documentation is mandatory for regulatory audits:
-
Mold Records: Batch number, fabrication date, and number of parts produced.
-
Resin Certificates: Material safety data sheets (MSDS) and biocompatibility test reports.
-
Process Logs: Vacuum pressure, curing time/temperature, and operator signatures .
Case Example: RapidDirect, a contract manufacturer, implemented a digital traceability system for vacuum casting. Each part is labeled with a QR code linking to its mold batch, resin certificate, and inspection results—enabling FDA audit compliance in < 1 hour .
Vacuum casting continues to evolve, driven by material advancements, process automation, and emerging clinical needs.
-
Bioactive Resins: Polyurethanes infused with antibiotics or growth factors for implantable devices, reducing infection risk .
-
4D Printing Integration: Shape-memory polyurethanes that respond to temperature or pH, enabling self-deploying stents or adaptive orthotics .
-
Sustainable Resins: Plant-based polyurethanes (e.g., soy-derived) that reduce environmental impact without compromising biocompatibility .
-
Automated Mold Fabrication: Robotic systems for silicone pouring and degassing, reducing human error and increasing consistency .
-
Digital Twin Technology: Virtual replicas of vacuum casting processes to optimize parameters (e.g., resin flow, curing time) before physical production .
-
AI-Powered Quality Control: Machine learning algorithms that analyze 3D scans of cast parts to detect defects faster than human inspectors .
-
Microscale Medical Devices: Vacuum casting of components < 1 mm in size for minimally invasive procedures (e.g., intravascular sensors) .
-
Organ-on-a-Chip Systems: High-fidelity microfluidic devices that replicate human organ function, used for drug testing .
-
Customized Cancer Treatments: Patient-specific drug delivery devices cast from 3D scans of tumors .
The combination of 3D printing (master models) and vacuum casting (end-use parts) is becoming more seamless:
-
In-Situ Master Model Fabrication: 3D printers integrated with vacuum casting systems, reducing lead time to < 24 hours .
-
Hybrid Parts: 3D-printed metal cores encapsulated in vacuum-cast biocompatible resin, creating strong yet lightweight implants .
Vacuum casting has established itself as a critical technology in medical device manufacturing, offering a unique balance of precision, flexibility, and cost-effectiveness. Its ability to produce high-quality, biocompatible parts in low to medium volumes makes it indispensable for prototyping, clinical trials, and niche end-use applications. From diagnostic equipment to prosthetics, vacuum casting enables innovations that improve patient outcomes and accelerate medical progress.
-
Partner with Specialized Manufacturers: Choose contract manufacturers with ISO 13485 certification and experience in medical applications (e.g., Materialise, RapidDirect).
-
Optimize Master Models: Use SLA 3D printing for complex geometries and CNC machining for smooth surfaces. Ensure masters meet final part tolerances, as vacuum casting replicates master accuracy .
-
Test Materials Early: Conduct biocompatibility and sterilization tests on resins before mold fabrication to avoid costly rework.
-
Plan for Post-Processing: Allocate time and budget for trimming, surface treatment, and assembly—critical for meeting clinical standards .
As healthcare continues to trend toward personalized, minimally invasive, and rapidly deployable solutions, vacuum casting will play an increasingly central role. Its ability to adapt to new materials, integrate with digital technologies, and meet stringent regulatory requirements ensures it will remain a cornerstone of medical device innovation for years to come.